
Cancer burden and control in China
Introduction
Cancer is one of leading cause of deaths in China, posing a great threat to resident health and causing huge economic burden. In recent years, trends in cancer mortality and incidence rates have shown increased. In 2015, there were about 3,929,000 cancer newly diagnosed cases with a number of 2,338,000 deaths (1). Compared with the data in 2013 year, a slight increase was observed in terms of cancer mortality and incidence (2). It is apparently that how to reduce cancer burden is more and more urgent. Researches suggested that a series of risk factors are related to such kind of diseases, particularly a growing aging and an extended life expectancy.
Actually, cancer prevention and control in China has achieved transient successful these years, by taking universal primary prevention aimed at adjusted risk factors, such as smoking control, healthy diet, and secondary prevention, especially in early detection and treatment. However, such effect could not be observed due to large population, ageing, and the short observation interval. Anyway, there is still a long way to go in cancer prevention and control in China.
This study is conducted to update epidemiology of cancer nowadays and summary preventive measures in China using available data extracted from previously published papers that has the potential to support information for improving policies on cancer prevention and control.
Global epidemiology of cancer
Based on GLOBOCAN 2018, it is estimated that 18.1 million new cases and 9.6 million deaths occurred worldwide, nearly one-half of the cases and over 50% deaths living in Asia in the year 2018. Incidence rates in males and females were 218.6 per 100,000 population and 182.6 per 100,000 population, respectively (3). The top five commonly diagnosed cancer types in males were lung cancer (14.5%), prostate cancer (13.5%), colorectal cancer (10.9%), stomach cancer (7.2%) and liver cancer (6.3%). Breast cancer (24.2%), colorectal cancer (9.5%), lung cancer (8.4%), cervical and uterine cancer (6.6%) and followed by thyroid cancer (5.1%) were more common in females correspondingly. The main causes of deaths were lung cancer (18.4%), colorectal cancer (9.2%), stomach cancer (8.2%), liver cancer (8.2%), breast cancer (6.6%) and esophageal cancer (5.3%) (4).
Epidemiology of cancer in China
Incidence
Nearly 3,929,000 (2,151,000 in male, 1,778,000 in female) cancer cases were newly diagnosed in 2015, which was equivalent of more than 10,764 cases diagnosed each day according to recent estimation by National Central Cancer Registry. The age-standardized incidence rates by Chinese standard population (ASIRC) and by world standard population (ASIRW) for all cancers combined were 190.64/100,000 and 186.39/100,000, respectively. The incidence rate was higher in men than in women (207.99/100,000 vs. 175.47/100,000) (1).
Distinct disparity in cancer incidence rate by regions was observed, which presented obvious geographical distribution features. Eastern China had the highest cancer incidence rate (316.03/100,000), followed by Central China (283.33/100,000) and cancer incidence rate in Western regions was lowest (249.51/100,000). After standardization, the sequence did not change although gap in different regions were narrowed. Lung cancer was the most common cancer in all regions (5). For all cancer combined, urban areas had higher incidence rate compared to its counterparts.
Mortality
About 2,338,000 cancer deaths (1,480,000 in male, 858,000 in female) were reported in 2015, corresponding to 6,405 persons died from cancer each day. Age- standardized mortality rates by Chinese standard population (ASMRC) and by World standard population (ASMRW) for all cancers combined were 106.72/100,000 and 105.84/100,000, respectively. Males had higher mortality rate compared to females (139.13/100,000 vs. 75.92/100,000) (1).
Mortality rate by regions was similar to incidence. Western areas had the lowest cancer mortality rate (103.55/100,000), behind Middle areas (112.32/100,000) and Eastern areas (104.14/100,000). Lung cancer was also the leading cause of death in all areas (5). When it comes to urban-rural difference, higher mortality rate was reported in rural areas in terms of age-standardized mortality.
Prevalence
Zheng et al. (6) reported that an estimated 5-year prevalence (thousands) for all cancers combined in 2011 in China was 7.49 million (3.68 million in male, 3.81 million in female). The proportion for 5-year prevalence (1/100,000) was higher in urban regions. When considering cancer types by sex, for men, 5-year prevalence was highest in stomach cancer, with estimated 0.62 million cases in 2011, followed subsequently by lung cancer, colorectal cancer, esophageal cancer, and liver cancer. For women, breast cancer had the highest 5-year prevalence, with estimated 1.02 million cases, followed by colorectal cancer, cervical cancer, thyroid cancer and lung cancer.
Survival
Population-based survival was estimated by Zeng et al. (7). Age-standardized survival in 2012–2015 was 40.5% (33.9% in men and 47.8% in women). It is estimated that urban areas had higher age-standardized survival (46.7%) for overall cancers combined than that in rural areas (33.6%). The age-standardized survival varied dramatically for individual cancers. The highest age-standardized survival was observed in thyroid cancer (84.3%) and pancreatic cancer had the lowest age-standardized survival (7.2%), for other cancers with relatively high survival (60%) in 2012–2015 including cancers of breast, bladder, uterus, kidney and prostate.
Trends in cancer incidence, mortality and survival
The age-standardized incidence remained stable on the period of 2000 to 2011 for men, while an increasing trend in age-standardized incidence was observed for women. For individual cancers by sex, it tended to display different change trends. For cancers of colorectum, lung, breast, cervix and uterine corpus had significant upward trend in age-standardized incidence in women. Especially, the incidence of thyroid cancer increased dramatically, even exceeding breast cancer in some places (Jiangsu province) in China (8). While in men, a growing trend in age-standardized incidence was seen for cancers of pancreas, colorectum, brain, prostate, gallbladder and leukemia, of which prostate showed fastest-growing. For both sexes, a decreasing trend in age-standardized incidence was seen in esophageal cancer, stomach cancer and liver cancer.
The Third National Retrospective Sampling Survey of Death Causes (9) suggested that mortality rate increased 83.1% compared to the First National Retrospective Survey of Death Causes and increased 22.5% compared to the Second National Retrospective Survey of Death Causes. In 1989–2008, crude mortality rate increased with 1.0% average annual percentage change, although mortality rate showed slightly drop after standardized by World stand population (10). Recently, a favorable trend was observed in age-standardized mortality rate which decreased significantly from 2000 to 2011 for both males and females (11).
Based on 72 local population-based cancer registries (2009–2011) and 22 registries (2000–2011), mortality and its trends were projected (3,11). An upward trend in age-standardized mortality rate was observed for cancers of colorectum, pancreas, prostate and leukemia in men, and for cancers of breast, cervix, and ovary in women, whereas age-standardized mortality rates from cancers of stomach, esophagus, and liver decreased dramatically for both sexes at the same time (11).
The age-standardized survival for overall cancers combined showed 9.6% increase from 30.9% in 2003–2005 (12) to 40.5% in 2012–2015. And in urban areas, it increased by 18.23% from 39.5% in 2003–2005 to 46.7% in 2012–2015, with 2.2% average change. In rural areas, age-standardized survival for patients with cancers showed greater growth compared with urban regions, that increased from 21.8% in 2003–2005 to 33.6% in 2012–2015, with 3.9% average change. The survival gap was narrowed between urban and rural areas over the period from 2003 to 2015. For both sexes, survival rate tended to be higher and rose rapidly in women whose age-standardized survival rate increased to 47.8% from 2003–2005 to 2012–2015. Although age-standardized survival also increased remarkably in men with 7.3% increase, it was 13.9% less than that in women in 2012–2015. In terms of different cancer types, half of them showed steadily increased over time only except for some lethal cancers, for example, pancreatic and gallbladder cancer (7).
Characteristics of epidemiology in China
Transition of cancer spectrum
The top 10 common cancers in China were lung cancer, stomach cancer, colorectal cancer, liver cancer, breast cancer, esophageal cancer, thyroid cancer, cervical cancer, brain cancer and pancreatic cancer (1). The Third National Retrospective Sampling Survey of Death Causes demonstrated that incidence of lung cancer, liver cancer, colorectal cancer and female breast cancer increased dramatically, and the largest growth rate was occurred in lung cancer. Over the past decades, it was estimated that the age-standardized incidence rate of colorectal cancer increased from 12.8 in 2003 to 16.8 per 100,000 in 2011, while the mortality rate rose from 5.9 to 7.8 per 100,000 (13). Similar to the United States (14), breast cancer was the most frequent cancer in women who tend to be considerably younger (45–55 years old) at diagnosis according to International Agency for Research (15). Cancer compositions in China were transiting to Western distributions gradually, which were characterized with high incidences of breast cancer and colorectal cancer, while cancers of esophagus and stomach were still common in China (16).
Variation of geographical distribution of cancer
Due to striking disparity of diet habits, socioeconomic status, living environment, and others, cancer incidence and mortality rates presented obvious geographical distribution, showing clustering. For lung cancer, a spatial analysis indicated that northeast regions had the highest mortality rate and northwest regions had the lowest mortality rates (17). Feicheng County (18) in Shandong province and Linzhou (19) in Henan province were the main high-risk areas for esophageal cancer. Gastric cancer was commonest in Gansu and Qing hai in Northwest China, followed by North China and Huaihe basin (20). Fang et al. reported that, at the provincial level, colorectal cancer mortality rate was highest in Eastern and Southeastern China, including Shanghai, Jiangsu, Zhejiang, Fujian and Guangdong provinces, followed by Northern China, such as Liaoning, Jilin and Heilongjiang provinces (21).
Cancer prevention and control
Primary prevention
Primary prevention means that, generally, we could decrease the probability of having cancer by reducing exposure to risk factors through taking a series of measures, including healthy diet, physical activities, before being cancer. Researches long-term suggested that risk factors related to cancer could categorize into uncontrollable and controllable factors. The former contains sex, age, family of history, and race. And controllable factors refer to unhealthy lifestyles, environmental exposure and so on. Chen et al. (22) reported that 23 potentially modifiable risk factors at the province-level using comparative risk assessment, the top three carcinogens were smoking, hepatitis B virus (HBV) infection and low fruit intake in males whereas they were low fruit intake, HBV infection and smoking in females.
Cancer has become a major public health problem in China, effective prevention and control is of great significance. In 2002, the National Central Cancer Registry Center was launched under the supervised of the Ministry of Health, making it possible to provide population-based cancer data and realize dynamic observation trends change of incidence, mortality and survival. To date, 574 cancer registries, with better data quality over time, were established among provinces within China. Additionally, the China Government has pushed a series of plans and policies on cancer prevention and control since 2012. Healthy China 2030 strategy, released in 2016 by the Communist Party of China Central Committee and the State Council, was designed to promote healthy lifestyles (23), which aimed to improve overall 5-year survival by 15%. The Mid-term and Long-term Plan for Prevention and Treatment of Chronic Diseases in China (2017–25) was issued based on Healthy China 2030 strategy in the beginning of 2017 to further the transition of disease treatment to health management autonomously (Table 1).
Table 1
| Year | Measures of cancer prevention and control |
|---|---|
| 2002 | National Central Cancer Registry Center was launched |
| 2002 | Neonatal Immunization Program (HBV vaccination) |
| 2005 | Early Detection and Early Treatment of Cancer in Rural Cancer |
| 2006 | Framework Convention on Tobacco Control Conducted Officially |
| 2007 | Early Detection and Early Treatment of Cancer in Huaihe River Basin |
| 2009 | Cervical Cancer and Breast Cancer Screening Program for Women in Rural Areas |
| 2012 | Early Detection and Early Treatment of Cancer in Urban Areas |
| 2012 | The Working Plan for Prevention and Treatment of Chronic Diseases in China (2012–2015) |
| 2016 | Healthy China 2030 strategy |
| 2017 | The Mid-term and Long-term Plan for Prevention and Treatment of Chronic Diseases in China (2017–2025) |
Meanwhile, the China Government also has implemented a great deal of actions to achieve such ambitious goal, such as tobacco control, promoting healthy lifestyles. Recently, great progress has acquired on tobacco control in China, although some key measures were underused (24). Additionally, in 2002, HBV vaccination was incorporated into Neonatal Immunization Program (Table 1) which could protect liver from hepatitis B virus infection effectively and reduce the liver cancer burden dramatically (25). A nationally HBV seroepidemiological survey conducted in 1992 showed that HBsAg carrier rate was 9.75% in the whole population, and in 2006, which declined to 7.18% for those people aged 1–60 (26). And the coverage of three doses of hepatitis B for infants and timely birth-dose coverage was 99.6% and 95.6% in 2015 (27), anyway, HBV infection has dropped significantly in the past three decades. In recent year, the introduction of prophylactic human papillomavirus (HPV) vaccination could diminish HPV infection efficiently, which also may reduce cervical cancer burden in the future. Next, how to improve awareness and attitudes towards of cancer prevention and vaccine application is extremely important. A survey was conducted in Yunnan province suggested that knowledge and awareness of HPV and the HPV vaccine was very low, with only 52.6% women known cervical cancer (28), especially for people with low education level.
Secondary prevention
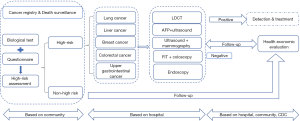
Secondary prevention, whose effectiveness has been certified in many countries, refers to early discovery, early detection and early treatment to mitigate the development of cancer. Mass screening on high-risk population and physical examination are the main ways for secondary prevention of cancer. It is suggested that implemented population-based cancer screening projects could reduce disease burden effectively. Mortality of colorectal cancer decreased by 50.70% from 28.6 (per 100,000) in 1976 to 14.1 (per 100,000) in 2014 due to the widespread use of colonoscopy (29). Similar effect was also seen in cancers of esophagus (30), stomach (31) and others (32,33). At present, in China, there are some National Cancer Screening Program (Table 1), which are Early Detection and Early Treatment of Cancer in Urban Areas (upper gastrointestinal cancer, liver cancer, colorectal cancer, lung cancer, breast cancer) (Figure 1), Early Detection and Early Treatment of Cancer in Huaihe River Basin (upper gastrointestinal cancer, liver cancer), Early Detection and Early Treatment of Cancer in Rural Cancer (upper gastrointestinal cancer, liver cancer, colorectal cancer, nasopharyngeal cancer, lung cancer), Cervical Cancer and Breast Cancer Screening Program for Women in Rural Areas, respectively, and Cervical Cancer Screening supported by Maternal Child Health (MCH) system (34). The ultimate aim of such screening projects is to find potential patients with cancer and all of them are available free.
Some questions are existed, for instance, low coverage rate, low follow-up rate and no effective cancer screening methods, although mortality rate of cancer declined dramatically is observed. Taking liver cancer screening for example, aimed at high-risk population with positive HBsAg, B ultrasound, coupled with a-fetoprotein (AFP) test was the main screening method, while it was considered as an inefficient screening method with low sensitivity and high-false positive rate (35,36), through decades of practical experience. Even for greater liver cancer, the effectiveness of diagnosis was only about 60%, which was difficult to target population-risk exactly. Furthermore, for some areas with relative lagging economy, it was hard to implement cancer screening.
To improve the effectiveness of cancer prevention and obtain better cancer screening outcomes, some key elements are needed urgently considered. First, to reduce the financial burden on the China Government funded system, how to define high-risk population more accurately is more important. In addition, we still lack a suit of proper and feasible screening schemes, which are suitable to national condition currently. And, current screening programs were far from sufficient to decline cancer mortality rate significantly. In order to improve quality of cancer screening, a series of measures are needed, such as using more precise biomarkers, increasing participate rate, and training the staff involving in cancer screening. Finally, screening effectiveness assessment methodology, combined with health economic evaluation, which is an important index for the intervention effectiveness of public health (37), should be improved. In brief, cancer screening in China still faces various challenge and opportunities, more investment and attention are deserved for the China Government and local population.
Tertiary prevention
Tertiary prevention primarily aims to reduce morbidity and disability, increase survival and improve quality of life for patients already diagnosed with cancer. Nowadays, most of therapy modalities are operation, chemotherapy, radiation. However, at the same time, it would also produce side effects for any piece of therapy modalities, such as vomiting, diarrhea, infection, even leukopenia (38). Moreover, people often suffer from cancer-related directly diseases, including pain, weakness, and wearing. Many cancer survivors had to bear levels of psychological burden inevitably. A meta-analysis pooled 52 studies used the DSM (Diagnostic and Statistical Manual of Mental Disorders) criterion of major depression suggested that prevalence of major depressive disorder and minor depression was 14.9% and 19.2%, respectively (39). Accordingly, how to alleviate psychological burden of patients deserves more attention for clinical workers.
The origin of such psychological burden for patients lies in lacking comprehensive, objective recognition of cancer that people usually tend to consider cancer can’t be cured or cancer is terrible. Such incorrect cognition will break patient’s self-confidence and even accelerate the development of cancer. Thus, it is the most important to help patients form a sound cognition, offering some psychological intervention such as psychological support (encouragement, conformation) or taking anti-depressant or other psychiatric medications if necessary, individual counseling with a professional may be the best way for cancer survivors (40).
In summary, cancer is one of the most important problems in China, although a series of measures were taken. China still faces great challenges on cancer prevention and control, such as geographical difference, cancer spectrum transiting to developed countries. Future effort should not only focus on mass screening programs, but also pay more attention to primary prevention and tertiary prevention.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Cancer Epidemiology for the series “Global Cancer Burden”. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ace.2019.08.02). The series “Global Cancer Burden” was commissioned by the editorial office without any funding or sponsorship. WQC served as the unpaid Guest Editor of the series and serves as the Editor-in-Chief of Annals of Cancer Epidemiology. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zheng RS, Sun KX, Zhang SW, et al. Report of cancer epidemiology in China, 2015. Zhonghua Zhong Liu Za Zhi 2019;41:19-28. [PubMed]
- Zheng R, Zeng H, Zhang S, et al. Estimates of cancer incidence and mortality in China, 2013. Chin J Cancer 2017;36:66. [Crossref] [PubMed]
- Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. In: Int J Cancer. 2018. Available online: https://gco.iarc.fr/today.
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Sun K, Zheng R, Zhang S, et al. Report of Cancer Incidence and Mortality in Different Areas of China, 2015. China Cancer 2019;28:1-11.
- Zheng R, Zeng H, Zhang S, et al. National estimates of cancer prevalence in China, 2011. Cancer Lett 2016;370:33-8. [Crossref] [PubMed]
- Zeng H, Chen W, Zheng R, et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health 2018;6:e555-67. [Crossref] [PubMed]
- Wei F, Wu Y, Tang L, et al. Trend analysis of cancer incidence and mortality in China. Sci China Life Sci 2017;60:1271-5. [Crossref] [PubMed]
- Ministry of Health, the People’s Republic of China. Report on the Third National Death Survey. Peking Union Medical College Publishing House, 2008.
- Zeng HM, Zheng RS, Zhang SW, et al. Trend analysis of cancer mortality in China between 1989 and 2008. Zhonghua Zhong Liu Za Zhi 2012;34:525-31. [PubMed]
- Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Zeng H, Zheng R, Guo Y, et al. Cancer survival in China, 2003-2005: a population-based study. Int J Cancer 2015;136:1921-30. [Crossref] [PubMed]
- Zhu J, Tan Z, Hollis-Hansen K, et al. Epidemiological Trends in Colorectal Cancer in China: An Ecological Study. Dig Dis Sci 2017;62:235-43. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. [Crossref] [PubMed]
- Fan L, Strasser-Weippl K, Li J-J, et al. Breast cancer in China. Lancet Oncol 2014;15:e279-89. [Crossref] [PubMed]
- Pan R, Zhu M, Yu C, et al. Cancer incidence and mortality: A cohort study in China, 2008-2013. Int J Cancer 2017;141:1315-23. [Crossref] [PubMed]
- Liu Y, Astell-Burt T, Liu J, et al. Spatiotemporal Variations in Lung Cancer Mortality in China between 2006 and 2012: A Multilevel Analysis. Int J Environ Res Public Health 2016;13:1252. [Crossref] [PubMed]
- Sun X, Zhao D, Liu Y, et al. The long-term spatial-temporal trends and burden of esophageal cancer in one high-risk area: A population-registered study in Feicheng, China. PloS One 2017;12:e0173211 [Crossref] [PubMed]
- Liu SZ, Yu L, Chen Q, et al. Incidence and survival of esophageal cancer with different histological types in Linzhou between 2003 and 2012. Zhonghua Yu Fang Yi Xue Za Zhi 2017;51:393-7. [PubMed]
- Zhou MG, Wang XF, Hu JP, et al. Geographical distribution of cancer mortality in China, 2004-2005. Zhonghua Yu Fang Yi Xue Za Zhi 2010;44:303-8. [PubMed]
- Fang JY, Dong HL, Sang XJ, et al. Colorectal Cancer Mortality Characteristics and Predictions in China, 1991-2011. Asian Pac J Cancer Prev 2015;16:7991-5. [Crossref] [PubMed]
- Chen W, Xia C, Zheng R, et al. Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health 2019;7:e257-69. [Crossref] [PubMed]
- Tan X, Zhang Y, Shao H. Healthy China 2030, a breakthrough for improving health. Glob Health Promot 2018;1757975917743533 [PubMed]
- Goodchild M, Zheng R. Tobacco control and Healthy China 2030. Tob Control 2019;28:409-13. [Crossref] [PubMed]
- Qu C, Chen T, Fan C, et al. Efficacy of neonatal HBV vaccination on liver cancer and other liver diseases over 30-year follow-up of the Qidong hepatitis B intervention study: a cluster randomized controlled trial. PLoS Med 2014;11:e1001774 [Crossref] [PubMed]
- Zhang S, Wang F, Zhang Z. Current advances in the elimination of hepatitis B in China by 2030. Front Med 2017;11:490-501. [Crossref] [PubMed]
- Liu J, Liang W, Jing W, et al. Countdown to 2030: eliminating hepatitis B disease, China. Bull World Health Organ 2019;97:230-8. [Crossref] [PubMed]
- Baloch Z, Yasmeen N, Li Y, et al. Knowledge and Awareness of Cervical Cancer, Human Papillomavirus (HPV), and HPV Vaccine Among HPV-Infected Chinese Women. Med Sci Monit 2017;23:4269-77. [Crossref] [PubMed]
- Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin 2017;67:177-93. [Crossref] [PubMed]
- Wei WQ, Chen ZF, He YT, et al. Long-Term Follow-Up of a Community Assignment, One-Time Endoscopic Screening Study of Esophageal Cancer in China. J Clin Oncol 2015;33:1951-7. [Crossref] [PubMed]
- Areia M, Carvalho R, Cadime AT, et al. Screening for Gastric Cancer and Surveillance of Premalignant Lesions: a Systematic Review of Cost-Effectiveness Studies. Helicobacter 2013;18:325-37. [Crossref] [PubMed]
- Sankaranarayanan R, Nene BM, Shastri SS, et al. HPV Screening for Cervical Cancer in Rural India. N Engl J Med 2009;360:1385-94. [Crossref] [PubMed]
- National Lung Screening Trial Research Team. Results of Initial Low-Dose Computed Tomographic Screening for Lung Cancer. N Engl J Med 2013;368:1980-91. [Crossref] [PubMed]
- Di J, Rutherford S, Chu C. Review of the Cervical Cancer Burden and Population-Based Cervical Cancer Screening in China. Asian Pac J Cancer Prev 2015;16:7401-7. [Crossref] [PubMed]
- Okajima W, Komatsu S, Ichikawa D, et al. Liquid biopsy in patients with hepatocellular carcinoma: Circulating tumor cells and cell-free nucleic acids. World J Gastroenterol 2017;23:5650-68. [Crossref] [PubMed]
- Xu RH, Wei W, Krawczyk M, et al. Circulating tumour DNA methylation markers for diagnosis and prognosis of hepatocellular carcinoma. Nat Mater 2017;16:1155-61. [Crossref] [PubMed]
- Shi JF, Dai M. Health economic evaluation of cancer screening in China. Zhonghua Yu Fang Yi Xue Za Zhi 2017;51:107-11. [PubMed]
- Schoenberg MH. Physical Activity and Nutrition in Primary and Tertiary Prevention of Colorectal Cancer. Visc Med 2016;32:199-204. [Crossref] [PubMed]
- Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 2011;12:160-74. [Crossref] [PubMed]
- Arch JJ, Vanderkruik R, Kirk A, et al. A closer lens: Cancer survivors' supportive intervention preferences and interventions received. Psychooncology 2018;27:1434-41. [Crossref] [PubMed]
Cite this article as: Cao M, Chen W. Cancer burden and control in China. Ann Cancer Epidemiol 2019;3:4.


